1. Different Systems, Different Stories
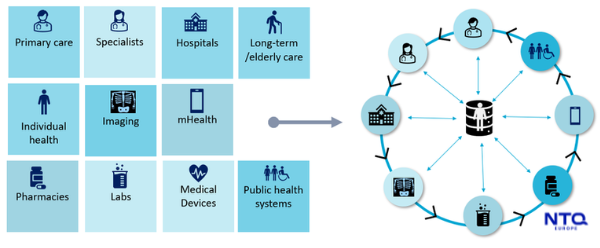
Healthcare data doesn’t break down because no one cares. It breaks down because everyone builds their puzzle piece at different times and with other priorities. A primary care clinic may use a simple EHR with limited integration. A specialist might use a standalone diagnostic system. A hospital might rely on a legacy patient management platform that hasn’t been upgraded in a decade. None of these systems was designed to work together, and they often don’t.
This disconnection creates silos. Lab results live in one place. Imaging data somewhere else. Medication history? Possibly still on paper, or locked in a separate pharmacy portal. In larger health systems, these silos multiply with every new acquisition, partnership, or location. For the people delivering care, it means delays. For the people receiving care, it means frustration.
What’s most troubling is that fragmented patient data in healthcare doesn’t just slow things down, it creates clinical risk. When providers can’t see the whole picture, they must rely on what’s available. That might mean missing an allergy, overlooking a past diagnosis, or repeating a test that was already done elsewhere.
2. The Patient Pays the Price
Patients feel the consequences of disconnected data systems more than anyone else. They’re asked to explain their history again and again, email lab results between providers, and bring printouts “just in case.” And in moments where time matters (like emergencies) these gaps become more than annoying. They become dangerous.
There’s also a growing emotional toll. When care feels disjointed, trust begins to erode. Patients lose confidence that the people treating them are working with accurate, up-to-date information. Even the most compassionate doctor is limited by what they can see; and when data is fragmented, what they can see is incomplete.
3. Why Interoperability Still Feels Out of Reach
With all the advances in cloud computing, APIs, and digital health platforms, why is healthcare data interoperability still challenging?
One reason is the lack of shared standards. Many systems are built around proprietary formats, which makes data exchange clunky or even impossible without custom development. Another is the diversity of regional policies. In Europe, privacy laws and health tech regulations vary widely between countries. What’s permitted in Sweden might be restricted in Italy or France.
Budget and capacity also play a role. Smaller clinics or rural providers often don’t have the resources (or the IT staff) to invest in integration. And even when funding is available, disrupting clinical workflows to implement new tech can feel too risky.

So, despite good intentions, many healthcare systems remain stuck in a patchwork of semi-connected platforms; each doing its job, but few working in sync.
4. Moving from Fragmentation to Connection
The good news is that full replacement isn’t the only path forward. Integration can happen gradually. Successful patient data integration efforts start with a clear audit: Where does data live? Who needs it? How often? What format? From there, teams can prioritize high-impact connections, like linking EHRs to diagnostic systems, or enabling cross-site data sharing for chronic care patients.
Modern solutions like middleware, data lakes, and FHIR-based APIs are making this easier. They allow health systems to preserve what works while improving what’s disconnected. Even a small step, like aggregating medication history across providers, can dramatically improve patient outcomes and team efficiency.
Of course, tech alone won’t fix it. It takes alignment across clinical, IT, and administrative teams, vendors willing to play fair, and leadership willing to look beyond short-term procurement cycles toward long-term care quality.

5. At NTQ Europe…
We’ve worked with healthcare clients across Europe who’ve faced this exact problem—scattered platforms, outdated systems, and growing pressure to modernize. Whether through EHR extensions, lightweight dashboards, or backend integrations, we help untangle fragmented ecosystems into usable, connected tools.
Fragmented patient data in healthcare isn’t just an inconvenience; it’s a barrier to safety, speed, and trust—and it’s worth solving, piece by piece.



















